Treatment Objectives
IBD Treatment
IBD Treatment – Inflammatory Bowel Disease
IBD treatment allows patients the ability to manage the disorder with less pain. Many of the medications available work to control the abnormal inflammatory response. By controlling the inflammation the intestinal tissues are given an opportunity to heal, decreasing the painful symptoms. Typically once symptoms of IBD are within a patient’s control, continued use of medications reduce the frequency of flare-ups and maintain remission.
Medications for the treatment of IBD
Medications are almost always the ‘first line’ for IBD treatment.
There are five main medicine categories:
- aminosalicylates – side effects may include nausea, vomiting, heartburn, headache and diarrhea.
- corticosteroids – side effects may include bone loss, diabetes, high blood pressure
- immunomodulators – side effects may include nausea, vomiting and headache
- biological agents – side effects may include the development of a life threatening infection, stomach pain, rash and nausea
- antibiotics – side effects may include nausea, vomiting and diarrhea
Over time, some people find that the medications do not offer the same result as it previously had. Some may have extensive and severe disease that is not easily controlled by the medications offered.
Surgery has often been the next option for IBD treatment. For those people suffering from severe ulcerative colitis, there is a way to cure the disease by surgically removing the entire large bowel. Other health issues can still remain regardless of a patient undergoing surgery.
Dietary Modification are recommended for the treatment of IBD
Dietary modifications are highly recommended for those suffering from IBD. Since the inflammation can perpetuate nutritional deficiencies, patients must be reminded to put thought into their food choices, and get as much nutritional support as possible. Doctors may also suggest:
Taking nutritional supplements
Avoidance of greasy, fried foods
Avoidance of cream sauces and meat
Avoidance of spicy foods
Avoidance of foods high in fibre
Medical Cannabis Treatment for Inflammatory Bowel Disease (IBD)
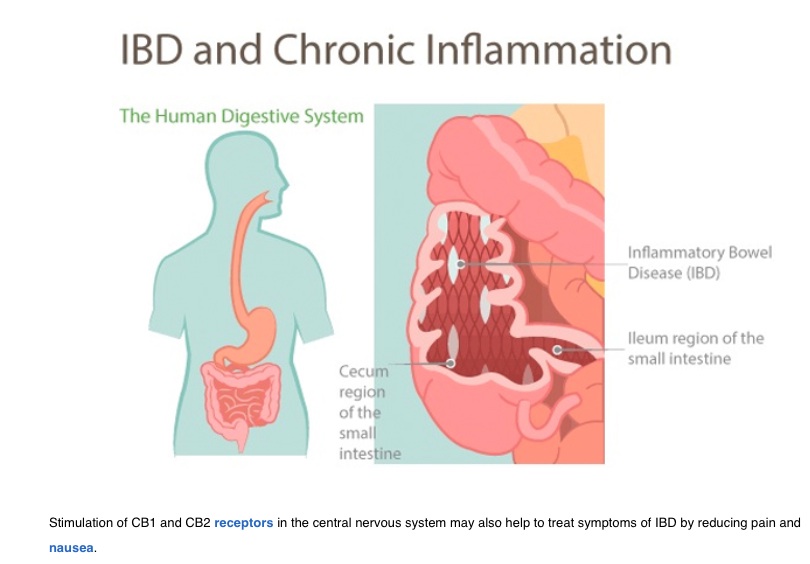
Cannabinoid receptors (CB1 and CB2) are found in the nervous system. This includes the enteric nervous system which has some part in controlling the function of the gut. The endocannabinoid system (ECS) has been studied and found to be essential in maintaining proper gut motility, sensation, and inflammation.
Though there are only a few studies that identify the impact of medical cannabis on patients with IBD, the evidence is mounting of its safe and efficient treatment for some patients. “A 2011 study found that 51% of ulcerative colitis patients and 48% of Crohn’s disease patients are lifetime cannabis users.”
Finding optimal treatment for Inflammatory Bowel Disease is imperative. These conditions are painful and diminish the quality of life for so many if not treated effectively. IBD treatment requires prevention of flare-ups to minimise continued pain and discomfort. Patients are reporting relief as a result of cannabis treatment.
IBD Statistics in Australia
- IBD affects an estimated 61,000 individuals at any given time.
- IBD is more prevalent in Australia than epilepsy.
- In 2005, more than 1,600 new cases of IBD were diagnosed in Australia.
- IBD affects approximately 1 in 250 people aged 5-40.
- Approximately 75,000 Australians have Crohn’s disease or ulcerative colitis and this statistic is projected to increase to 100,000 by 2022
What is IBD?
Inflammatory bowel disease (IBD) is a medical term and it describes a group of conditions where the intestines experience chronic inflammation and swelling. Because of this prolonged inflammation, parts of the digestive tract become damaged. Two major types of IBD are Crohn’s disease and Ulcerative colitis. Ulcerative colitis affects the surface layers of the large intestine (colon) whereas Crohn’s disease can occur in any part of the digestive tract from the mouth to the anus. Crohn’s disease inflames the entire thickness of the intestinal wall.
IBD is a very individual disease with symptoms dependent on where the disease is located in the gastrointestinal tract and how severe the inflammation is within the affected area. IBD is a chronic condition, though symptoms tend to wax and wane with intensity.
Symptoms of IBD:
- abdominal cramps and pain
- frequent, watery diarrhoea (may be bloody)
- severe urgency to have a bowel movement
- fever during active stages of disease
- loss of appetite and weight loss
- tiredness and fatigue
- anaemia (due to blood loss)
For some people with IBD they experience problems that fall outside of the gastrointestinal tract. This includes pain within the joints, certain skin conditions, ocular inflammation, liver disorders and osteoporosis.
Causes of IBD
- Idiopathic Disease – Researchers have not yet defined a cause for IBD.
- Potentially a combination of genetic, environmental and immunological factors.
- Exposure to triggers from the environment such as viruses, bacteria. Something that activates the immune system for its normal defence mechanism (inflammation) against a foreign substance.
- In most people, this immune response gradually diminishes once the foreign substance is destroyed. In those with a genetic susceptibility to develop IBD, the immune system continues failing to react to the switch off signals.
- Prolonged inflammation will eventually damage the walls of the gastrointestinal tract. This is what causes the symptoms of IBD.
What is the difference between Inflammatory Bowel Diseases : Crohn’s Disease versus Colitis?
- Crohn’s disease can be located anywhere in the GI tract
- Inflammation is oftentimes “transmural”
- Patients of Crohn’s experience more complications such as fistulas, strictures, and obstructions.
versus
- In Ulcerative Colitis, the inflammation is exclusively in the colon (large intestines).
- It is generally in one continuous patch
- Colitis has a smoother appearance
Clinical Studies / References: